Information for Teachers: Children Who Wet And Soil
What is enuresis?
Enuresis is the involuntary discharge of urine. It is considered to be a problem after the age of five by which time it is generally accepted that bladder control should have been established.
Children with daytime wetting characteristically feel the urge at the last minute or can try and hang-on for too long and may suddenly demonstrate holding postures e.g. ‘curtsey’ using their heel to stop the flow of urine.
Daytime wetting happens for around 3-4% of children between the ages of 4 and 12, and it is twice as common in girls. (Lane and Robertson, 1997). Two-thirds of these children experience combined day and nighttime wetting. It is important to address the daytime wetting first.
Some children may have underlying physical problems such as an unstable bladder – where the detrusor muscle around the bladder is overactive and causes the bladder to contract and empty before it is full, resulting in either wet underpants or multiple trips to the toilet.
What is faecal incontinence?
Faecal incontinence is the medical term for soiling in children over the age of 4 years. In most cases, faecal incontinence develops as a result of long-standing constipation (Proctor and Loader, 2003). It is estimated that constipation occurs in up to 10% of children (Leung et al, 1996).
The build-up of poo in the bowel and rectum results in the bowel getting so stretched that it is unable to register that there is a poo. As a result the usual signal to the brain that a child needs to go to the toilet is not sent and often the poo comes out catching the them unaware. We call this “sneaky poo”.
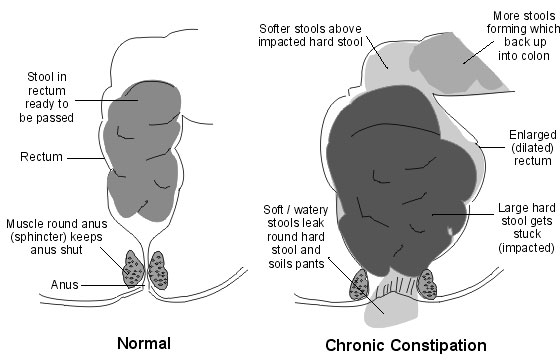
Sneaky poo is new, soft poo that moves down the bowel oozing around the hard poo and trickling out. Children with faecal incontinence often wet (day and/or night) as the constantly full rectum affects bladder functioning. Urinary tract infections as a result of this are also common.
In most cases, the child is not aware that this happening. They are not being lazy and punishment will not help solve the problem.
How can teachers help?
- Involve the Public Health Nurse assigned to the school. Parental consent must be obtained first.
- Support children in your class to drink at regular intervals.
- Get to know the child and their family. Discuss the particular needs of the child with the parents. Will they put spare clothes, wipes and a plastic bag in the child’s bag? What help does the child need with cleaning themselves up? Put a plan in place for dealing with wetting/soiling episodes – is there a support person prepared to help clean the child up or should the teacher phone the parents?
- Keep in touch with the parents using a daily notebook or communication diary.
- In discussion with the parents, support a toilet routine/management plan for the child during the school day. This may involve a discrete signal from the child indicating that they need to go to the toilet. Check on the child if they have been absent for longer than usual.
- Look out for signs that the child may need to go to the toilet – holding postures, playing with pants etc.
- Make sure that the toilet environment is private; that other children cannot look over or under the partitions, and check that door locks work. Check that toilets are warm, clean and have toilet paper and hand towels.
- Send a “toilet buddy” with the child if necessary.
References:
“How Teachers can help” abridged from Bowel Group for Kids Incorporated www.bgk.org.au
Lane, M and Robertson, MD “Diurnal Enuresis” Paediatrics in Review Vol 18(12) Dec 1997
Leung, AK, Chan, PY, Cho HY “Constipation in Children” American Family Physician 1996 Aug 54(2) 611-8, 627
Proctor, E and Loader, P “A 6-year follow up study of chronic constipation and soiling in a specialist paediatric service” Child: Care, Health and Development” 29 (2) 103-109
 |
 |