Toilet Training for Children with Autism Spectrum Disorders, and Learning Disabilities
Toileting with Disability
Children with autism spectrum disorders are more likely to have bowel difficulties, ranging from loose poos to constipation. Children with other conditions such as Down Syndrome are known to be more prone to constipation.
Development of bladder/bowel control
- Infant – the bladder/bowel empty automatically when full
- 1-2 years - gradual awareness of fullness
- 3 years – the ability to hold on
- 3-4 years – can initiate daytime emptying of bladder or bowel
- 6 years – able to start urination at any level of bladder filling and initiate defecation at an appropriate time or place
Children with learning disabilities need more help to master toileting skills. It is important to toilet train according to developmental age, not physical age.
Unless a severe neurological deficit is present a toilet training programme is recommended for all children, undertaken with a trained continence professional and adapted to suit the degree of disability. All children can be trained to some level.
When toilet training children with autism spectrum disorders or learning difficulties it is important to have a plan, be consistent and patient, give calm responses and praise desired behaviours.
First steps
- Contact your local continence advisor. Find them here.
- Keep a chart of wetting and soiling. Look for a pattern.
- Assess what skills the child already has e.g. being able to pull up/down pants, sit on toilet without help, wash hands.
- Assess what special difficulties the child has e.g. short concentration span, difficulty following instructions. Resolve these by using music, sticker charts, food colouring in the toilet water, ping pong balls in the toilet bowl, favourite songs or an ‘interest’ bag.
- Remove nappies, or use nappies that enable a ‘wet’ sensation.
- Use the chart to determine the best time to use the toilet, then take the child to the toilet when they are most likely to do wees/poos. After meals is best as the food and drink stimulate the gastrocolic reflex which moves digested food through the system.
- Assess the environment. If the child doesn’t like open/enclosed spaces adapt the environment accordingly. See the toilet through the eyes of the child e.g. if the child doesn’t like toilet flushing, wait until they are away from the toilet first or add some food colouring to the tank water. Put some toilet paper in the bowl to avoid splashback.
- Break down the toileting process into small steps giving clear instructions:
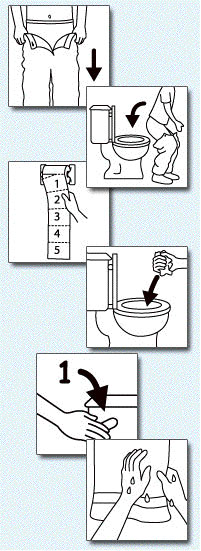
1. Pull down pants
2. Sit on toilet
3.Use the toilet
4. Wipe bottom with paper
5. Pull up pants
6. Flush toilet
7. Wash hands
- Start one step at a time and add additional steps over time. Praise each step. Children without disabilities pick up on body language, but children with autism spectrum disorders and learning disabilities need simple, clear language around going to the toilet.
- A rewards/star chart can be used if appropriate. Try not to use ‘bribes’ as such but make the reward a game or time with you.
Children who will only poo in a nappy
The first step is to get child to poo in the nappy in the toilet/bathroom. Then progress to sitting on the toilet wearing the nappy.
Once this is established as a behaviour gradually cut out the seat of the nappy, so that when they ‘go’, the poo falls into the toilet (yet they retain the feeling of having the nappy there). Gradually cut away more and more of the nappy over time (it can be messy with the absorbent crystals) till you end up with them wearing just the waistband.
Every time they ‘go’, praise them for their efforts.
Resources
New Zealand Toilet Map
Apply for a Toilet Card
Useful charts
Websites
ERIC (Education and Resources for Improving Childhood Continence)
SPELD NZ
NZ Down Syndrome Association
Autism NZ
Autism Speaks
Sources:
Treatment and Education of Autistic and related communication- handicapped children
“We can do it!” Helping children who have disabilities with bowel and bladder management” ERIC
 |
 |