Faecal Incontinence (Soiling)
What is Faecal Incontinence?
Faecal Incontinence is the medical term for soiling in children over the age of 4. In many cases, it develops as a result of long-standing constipation (Proctor and Loader, 2003). It is estimated that constipation occurs in up to 10 percent of children (Leung et al, 1996).
The build-up of stool in the bowel and rectum results in the bowel getting so stretched that it is unable to register that there is a poo. As a result, the usual signal to the brain that they need to go to the toilet is not sent and often the poo comes out catching the child unaware. We call this “sneaky poo” or new, soft stool that moves down through the bowel oozing around the hard stool and trickling out.
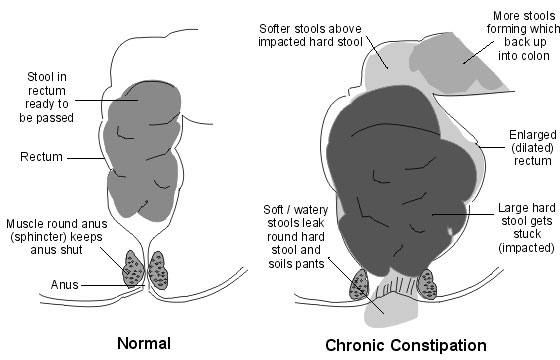
If the constipation is severe, it may seem like your child has diarrhea, as they may pass runny or loose bowel motions. This is because the plug of hard stool obstructs the passage of normal bowel motions, and the loose or runny stool passes around it.
In most cases, the child is not aware that this happening. They are not being lazy and punishment will not help solve the problem.
Urinary symptoms such as daytime and/or nighttime wetting, or urine infections as a consequence of constipation or soiling, can be common.
Management:
First steps:
- Discuss the problem with your child. Reassure them that they are not the only one with this problem, and that with their cooperation it can be fixed.
- There are a variety of books on the topic, such as “Poo Hoo” (available from Continence NZ) that you can read with your child. Other resources can be found at the public library, internet such as Continence NZ website or Kidshealth, or making contact with Continence NZ.
- Take your child to your GP. The doctor will need information about your child’s diet and fluid intake, frequency of soiling, triggers to soiling, and types of bowel motions they are passing. They will probably feel your child’s abdomen (tummy) to see if they can identify any lumps of stool. Based on their findings, a laxative may be prescribed to soften the bowel motion and keep it soft to allow your child’s rectum to return to its previous tone or normal state.
- In some cases, the doctor may also recommend a referral to a pediatrician.
- Contact your local continence advisor for further support and information. See the “Continence Service Providers” section of the Continence NZ website to find an advisor in your area.
- If your child attends school contact the Public Health Nurse affiliated with the school (ask at the school office or ring your local Public Health Unit). Public Health Nurses can help with education, resources, toileting programs, and support for you and your child.
The general rule of thumb is that it will take AT LEAST as long to resolve the problem fully as it did to get constipated, so plan to be managing constipation for months at best, to several years at worst.
Treatment
The goal of treatment is to empty the large intestine and rectum.
This is done using softening and stimulating laxatives, which may initially be at frequent, high doses. It will be messy initially as the old stool comes out so it is best to keep the child home from school while this part of the treatment is carried out.
To establish regular bowel movements:
- Maintain a regular daily dose of laxatives as prescribed.
- Encourage your child to sit on the toilet 10 – 15 minutes after eating (eating activates the gastro-colic reflex which stimulates faeces to move through the bowel),
- Encourage your child to use a foot stool to support their feet while sitting on the toilet, and lean forward with their elbows on their knees (this opens up the pelvic floor muscles and allows the bowel motion to pass out more easily).
- Gentle blowing such as a balloon or bubbles can further assist the poo passage.
- Keep a record of types and frequency of bowel motions.
- Ensure your child is drinking regularly through the day.
- Encourage your child to eat from all the food groups to maintain regular easy to pass bowel motions.
- Encourage your child to have some exercise daily. This also helps stimulate movement of faeces through the bowel.
It is important to maintain regular bowel movements long term by using maintenance doses of laxatives, (the dose can be adjusted as needed, usually in consultation with your doctor).
Be alert for signs that the child is becoming constipated again – increasing flatulence (passing wind), bad breath, soiling underpants, urinary tract infection and sore tummies.
Commonly Used Laxatives
Lactulose
Lactulose softens hard poos making them easier to pass. It works well in mild to moderate constipation. It is not effective on its own in severe constipation when there is a large amount of hard poos backtracking up the colon, but is often used in conjunction with other laxative medications.
Movicol
Movicol can be used in all stages of treatment, but particularly for initial disimpaction. The dose will be adjusted as required to maintain regular bowel motions.
Toilet Routine
Maintaining a regular toileting routine is important. Encourage the child to sit on the toilet 15-20 minutes after breakfast, lunch and dinner when the gastro-colic reflex is active. Allow enough time for children who attend childcare or school to sit on the toilet before you leave home. Praise/reward the act of sitting on the toilet rather than just results.
Diet and Fluids
Encourage:
- Adequate fluid intake or approximately six evenly spaced drinks of water or water based cordial a day.
- 5+ a day servings of fresh fruit and vegetables. Try a “pirate’s” or “princess’s” platter with vege sticks (e.g. carrot, zucchini, celery, capsicum, cauliflower) with dip, and seasonal sliced fruit (e.g. apples, pears, plums, pineapple) for morning or afternoon teas.
Exercise
Children aged 5-18 should:
- Undertake 60 minutes or more of moderate to vigorous physical activity throughout each day;
- Be active in as many ways as possible; for example, through play, cultural activities, dance, sport and recreation, jobs around the home.
- Be active with friends and whānau, at home, school, and in your community.
- Spend less than two hours a day (out of school time) in front of television, computers and game consoles.
(Guidelines from Sport and Recreation NZ - www.sparc.org.nz)
References:
Proctor, E and Loader, P “A 6-year follow up study of chronic constipation and soiling in a specialist paediatric service” Child: Care, Health and Development” 29 (2) 103-109
Leung, AK, Chan, PY, Cho HY “Constipation in Children” American Family Physician 1996 Aug 54(2) 611-8, 627
 |
 |